MULTI-ACT from the health care manager perspective
The MULTI-ACT project is in the final stages of developing a key component of the research and innovation documentation infrastructure to ensure effective and outcome-orientated cooperation between all stakeholders through a new Collective Research Impact Framework. In this blog post we’ll reflect on its use for health care managers.
What is the problem MULTI-ACT is trying to address?
We all know that researchers, patients and health care managers speak different languages, talk about different things and anticipate different outcomes when they consider research and innovation. Bringing all stakeholders together and teaching them to speak with each other rather than to each other is an important part of creating lasting and effective innovation in health care. This is particularly critical when it comes to providing health care solutions to patients with brain disease. Patients with brain pathologies present particular challenges to doctors, care workers as well as researchers trying to develop innovations to improve their care outcomes.
What is the solution MULTI-ACT offers?
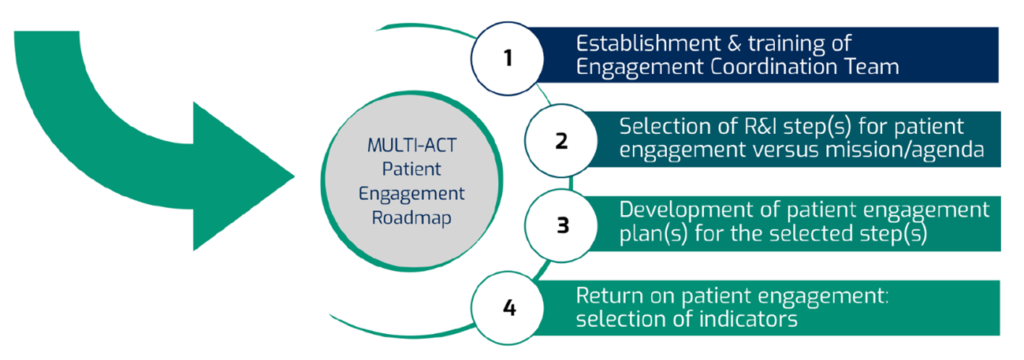
MULTI-ACT appears to have stepped into this important field with the ambition to create guidance for all stakeholders to facilitate effective cooperation between patients and those professionally engaged with their care and researchers. MULTI-ACT aspires to produce tools based on a new model of effective cooperation including detailed guidance facilitating a 4-step care pathway. Scorecards are developed in parallel to this, helping all stakeholders to base their actions on shared values, identified patient needs and expectations. This aligns with the key requirements of all modern and progressive health care: to be patient centred, supportive and guided by the values of compassion, care and deliver this in a collaborative spirit to achieve holistic care outcomes.
The issue of patient engagement in decision-making
I would like to focus my comments below on the intricate issue of patient engagement which present particular challenges to health care staff in this field. Shared decision making is now a key criterion of high-quality health care delivery. We know that is results in better decisions, improved health care outcomes and increased medication compliance and lower care pathway attrition rates.
However, the barriers to implementing shared decision making remain huge. Even today, medical students are still inculcated with a deep belief in the superiority of medical evidence-based knowledge. Patient perspectives are still routinely neglected or delegitimised in patient doctor conversations. Yet, we know that holistic and effective health care can only be delivered when patients feel part of the solution. Their commitment to the health care packages depends on them feeling that their concerns, reservations and ideas about what constitutes good health care are being taken seriously. This often jars with what doctors think about their health care based on scientific evidence and detailed professional medical knowledge. Patient doctor encounters are too often still a clash between different perspectives, different cultures and different visions of what constitutes good care. MULTI-ACT provides the building blocks to build the bridge between all stakeholders when constructing efficacious care packages for patients with brain disease. It pays particular attention to the issues around patient engagement in research and provides a useful framework structuring patient engagement activity for researchers and clinicians. Its roadmap including four steps for patient engagement is instructive for everyone involved (see below).
It ensures meaningful engagement of patients in the process of innovation and locates MULTI-ACT’s facilitation work clearly in the upper rungs of Arnstein’s ladder of participation which is a widely accepted measure of patient involvement (Kaehne, Bray and Horowicz, 2020).
The project however also develops strategic management tools such as the MASTER Scorecard which allow stakeholders to demonstrate the potential impact of the innovations and initiatives for patient care. This builds the link between the innovation itself, grounded in shared decision making based on meaningful patient engagement, and the implementation phase where it is essential for managers to assess the impact on patients. Too often care innovations are well meaning and may prove to be effective but have little impact on patient’s life as their implementation is not assessed in the long term. MULTI-ACT provides a unique mechanism to support managers in the innovation cycle from inception, patient engagement all the way to post-implementation analysis.
It thus provides a unique tool to improve patient centred care for people with brain diseases that will be immensely useful for managers and health care providers in the future.
This blog was written by Dr Axel Kaehne, President EHMA, Reader in Health Services Research, Medical School, Edge Hill University
REFERENCES
Kaehne A, Bray L and Horowicz E. (2020). Co-producing health care – pragmatic principles and an illustration. Emerald Open Res 2020, 2:10 https://doi.org/10.35241/emeraldopenres.13475.2).


